VULVODYNIA
What is it?
VULVA: designates the external area of the female genitalia. The vulva encompasses the: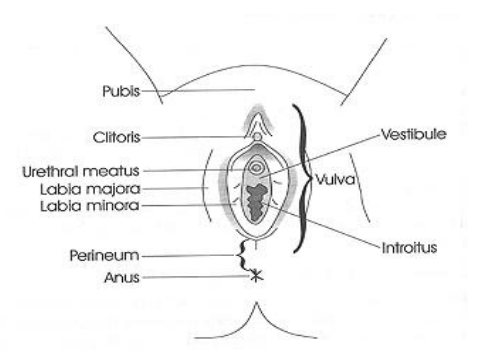
- Clitoris
- Opening of the urethra (urethral meatus)
- Opening of the vagina (vestibule)
- Labia minora
- Labia majora
DYNIA: refers to pain
VULVODYNIA means painful vulva. There can be pain in specific areas of the vulva or diffuse vulvar pain.
How do I know if I have vulvodynia?
Vulvodynia is a diagnosis of exclusion. Your GP and/or specialist will help rule out other causes for vulvar pain (eg skin conditions; vaginal infections; sexually transmitted infections; factors associated with childbirth and vaginal delivery etc).
Vulvodynia is usually diagnosed when:
-
- Other conditions are ruled out (however sometimes other conditions may co-exist with vulvodynia – eg skin conditions)
- Pain has been present for longer than 3 months in the area of the vulva
Causes
There is no known single cause of vulvodynia; what we do know however, is often a number of factors combine to make the perfect storm which can result in vulvodynia. Associated factors include:
- Other painful conditions such as irritable bowel syndrome, endometriosis, painful bladder syndrome (interstitial cystitis), etc
- Hormonal changes related to menopause or medications (eg chemotherapy)
- Ongoing inflammation following vaginal infections (eg thrush, bacterial vaginosis etc)
- Genetic pre-disposition
- Psychological factors: stress, physical/psychological trauma, depression/anxiety etc
- Constant pain in any area of the vulvar which may be aggravated by sitting, underwear, tight clothing, exercising etc
- Intermittent pain in the vulvar which is only aggravated by direct touch such as attempting to insert a tampon, a finger or with sexual intercourse
- Painful intercourse (also known as dyspareunia)
Physiotherapy Assessment (often requires 2 sessions)
- Information gathering: discussion with you to obtain a detailed history of your symptoms and related factors. This consultation may also include real time ultrasound to image your pelvic floor muscles and provide feedback for you.
- Physical assessment: Alchemy in motion pelvic health physiotherapists have extra training and experience with detailed assessment of the pelvic floor. This usually involves a vaginal examination to assess the contribution of your pelvic floor muscles to your symptoms.
Although this is an important part of your assessment – this will not be undertaken unless you provide consent. We understand the sensitive nature of this physical assessment and will not go ahead unless you are completely comfortable.
Physiotherapy Treatment
Physiotherapy treatment is based on the findings from your initial assessment and will be tailored to your individual needs and goals, this may include:
- Gentle and progressive desensitisation techniques for sensitive skin and muscles
- Gentle manual therapy to release overactive and tight muscles including pelvic floor muscles
- Education to demystify your symptoms with a heavy emphasis on explaining your pain
- Education to improve vulvar care; bladder and bowel habits and sexual function
- Prescription of a home exercise program
The ultimate goal of physiotherapy is to empower you with knowledge, get you back to the things you enjoy and finally, to improve your confidence with self-management.
Other Treatment Options
- Medication prescribed by your GP and/or Gynaecologist – see here for further information https://www.pelvicpain.org.au/category/medications/
- Special Pain Psychologist
- Sexual Counsellor
- Dietician
- Exercise Physiologist / Movement Coach


